Cancer Symptoms & Treatment
CANCER SYMPTOMS & TREATMENT (IN BRIEF)
Receiving a diagnosis of cancer presents numerous challenges: learning about your disease, selecting the physicians who will care for you, and making decisions about your treatment. Then come the day-today challenges: integrating the treatment schedule into your life, coping with the symptoms and side effects of the treatments, and finally making the transition to being a cancer survivor.
We hope our texts will provide information and support to help you in meeting these challenges. We have included information about cancer and cancer treatment, but the focus is on managing the symptoms of the disease and the side effects of treatment. Equally important is information we hope will help you and your family cope with the emotional and practical concerns that come up during this time.
(11) Cancer Symptoms & Treatment

What can I do for flu-like symptoms?
Flu-like symptoms may be caused by infection, cancer, or treatment for cancer. These symptoms are most commonly fever, chills, aches and pains in the muscles (myalgias), and fatigue. You might also experience decreased appetite, headache, nausea, vomiting, or diarrhea.
If you develop these symptoms, call your doctor or nurse. Always immediately report fever of 100.5ºF or greater, with or without chills, to your doctor’s office unless the fever is a known chronic problem. If these symptoms are new, you need to make sure you don’t have an infection. The doctor will ask you questions, perform a physical examination, take blood samples, and perhaps perform other tests. If you have an infection, treatment will be prescribed.
When a cancer causes flu-like symptoms, they are commonly referred to as tumor fever. Many people with tumor fever experience symptoms on a daily basis and usually at the same time (or times) each day. Very often, when treatment of the cancer results in remission or cure, tumor fever goes away.
Certain treatments for cancer can cause flu-like symptoms. If these symptoms are likely to occur from your treatment or from other medications, your doctor or nurse will tell you. The reaction can occur while you are receiving the medication, within a few hours, or even several days after the treatment.
Flu-like symptoms can be caused by:
• Chemotherapy, such as gemcitabine, dacarbazine, and bleomycin.
• Biologic therapy (therapy that boosts your immune system to fight the cancer), such as interferon or interleukin, and monoclonal antibodies, such as rituximab and trastuzumab.
• Medicines to strengthen bone, such as pamidronate and zoledronic acid.
If you are likely to experience these symptoms while you are receiving the medication, the doctor or nurse will give you premedication (before the treatment) to prevent the reaction: acetaminophen, diphenhydramine, nonsteroidal anti-inflammatory medication (ibuprofen, naproxen), or even meperidine or morphine.
If you experience flu-like symptoms at home, regardless of the reason, the following measures may help:
• Your doctor may prescribe acetaminophen or nonsteroidal anti-inflammatory medicines (e.g., naproxen) for you to take around the clock (on a regular basis).
• Drink plenty of fluids to prevent dehydration from fever.
• Take cool to tepid sponge baths to keep your fever down.
• Take regular uninterrupted rest periods if you are tired.
• Ask your doctor to prescribe medicine for nausea, vomiting, and diarrhea if you develop these.
What can I do to treat itching?
Itching is a sensation that makes people want to scratch. The medical term for this is pruritus. Itchiness can occur on one area of the body (localized), or it can affect the entire body (generalized). It may also be accompanied by a rash or other skin changes. In patients with cancer, itching can have a number of causes:
• Some cancers, including leukemia, lymphoma, and cancers of the stomach, lung, or breast, may be associated with itching.
• Some chemotherapy medicines may cause itching, such as doxorubicin and erlotinib.
• Radiation therapy may cause skin changes, including itching. If you are being treated with radiation, contact your doctor or nurse before applying anything new to your skin to soothe irritation.
• Some medicines, including pain medicine (narcotic analgesics like morphine) and antibiotics can cause itching.
• An allergic reaction to medicine can cause itching.
• Other diseases, such as liver disease and kidney failure, may be associated with itching. ( Jaundice is characterized by a yellowing of the skin and the whites of the eyes resulting from a buildup of bilirubin in the tissues; it can occur if the bile ducts are blocked or if the liver is not functioning, and is accompanied by a darkening of the urine and a lightening of stool color.)
• Other causes are dry skin, insect bites, and changes in the soap or laundry detergent.
Constant scratching can cause more irritation to the skin and, in some people, a break in the skin that can bring about additional discomfort and even infection.
Itching can interfere with your sleep and overall quality of life. If you have itching, a rash, redness, or breakdown of your skin, contact your doctor or nurse before applying anything to your body. The doctor will ask you many questions, inspect your skin, and possibly take a blood sample. Be prepared to give them the following information:
• The area that is affected, when it started, and what makes it better or worse
• Medicines that you are taking, including prescription and over-the-counter medicine (Be sure to tell them about any new medicines.)
• Changes in your skin, such as rash, hives, or dryness, and changes in the color of your skin, such as redness or yellow skin (jaundice)
If the cancer is causing the itching, treatment resulting in remission or cure often stops it. If the itching is caused by a medicine, your doctor may stop the medicine or switch to another one that won’t cause itching. If you have itchiness or a skin reaction from radiation treatments, speak to your nurse about specific skin recommendations for people receiving radiation therapy.
There are many treatments for itching. Here are some general measures that almost anyone can try:
• Bath or shower using tepid water and a super fatted unscented soap (e.g., Dove). Aveeno oatmeal baths may also be soothing.
• Use emollient lotions, such as Curél or Lubriderm.
• Keep your fingernails trimmed.
• Keep the air humidified.
• Drink plenty of fluids.
• Wear loose-fitting cotton clothing; use cotton sheets.
• Apply cool compresses for localized itching.
• Use distraction measures, relaxation techniques, or guided visual imagery.
Your doctor or nurse might suggest other treatments:
• Steroid creams, either by prescription or over-the counter;
• Topical or oral antihistamines (e.g., diphenhydramine);
• Sedatives for those who are unable to sleep;
• Referral to a dermatologist for a consultation.
Lisa’s comment:
Pruritis associated with the radiation field drove me crazy. Even though I used all recommended creams (Biafine, Bactroban Ointment, Betamethasone Dipropionate Ointment),
I still found myself scratching absentmindedly. I felt that I needed to put myself in mittens, in addition to keeping my fingernails short, in order to prevent significant skin breakdown.
ACTIVITY AND SLEEP
I feel tired much of the time. What can I do to increase my energy?
Lisa’s comment:
I am a single professional woman. I have elderly parents who live across town, a brother who lives 15 miles away, and numerous friends who live both near and far. I am an independent individual. I insisted on getting myself to and from my treatments (chemotherapy) via mass transportation, alone-I live about 30 miles from the Cancer Center.
My fatigue was significant, but generally occurred a few days after treatment. My parents and friends wanted to drive me to my treatments, but I wouldn’t allow them. My mother, therefore, took on the added chore of doing my laundry and food shopping every week. My parents’ help significantly contributed to my increased energy levels. It allowed me to save my energy for long workdays.
Mary Ann’s comment:
I wish I had the magic answer as to what to do about the fatigue that accompanies my treatment. I, too, am tired all the time. I was doing a whole lot of napping but have now tried pushing through that 3 o’clock (or 10 a.m., 11 a.m., 2 p.m., 4 p.m., 6 p.m.-anytime) exhaustion. Sometimes it works, sometimes it doesn’t. Caffeine is not the answer and I find myself drinking Gatorade of all things! I always thought of it as some fancy Kool-Aid but have discovered, thanks to the advice of my oncologist, that it does add something back to your system. It really has helped me (and it comes in a low-calorie variety but good luck finding it!)
Fatigue is a common problem for people with cancer.
You may feel tired, weak, or weary; lack energy; be unable to concentrate; or feel irritable or depressed.
Many things may cause fatigue:
• The disease itself
• The treatment you are receiving
• The side effects of certain medications (e.g., medications to treat pain or nausea)
• Anemia (a low red blood cell count)
• A decrease in the amount of food you eat
• A decrease in the amount of liquids you drink
• Difficulty sleeping
• Emotional distress
• Chronic pain
However, many people with cancer develop fatigue without any clear single cause.
Sleeping extra hours at night, by going to bed earlier or staying in bed a bit later in the morning, will improve your energy. Resting during the day is also important: napping for short periods or just lying down and relaxing. Plan these rest periods for times when you know you will be more likely to feel tired.
Even bathing, dressing, or eating may cause some people to feel tired, and they should plan time for a short rest after these activities. However, at the same time, you want to push yourself to be as active as possible.
Lying in bed all day generally makes you weaker. In fact, there is evidence that exercising will actually increase your energy level as long as you don’t push yourself to the point of exhaustion. If you are currently exercising on a regular basis, try to maintain your schedule, adjusting the intensity and frequency of your exercise regimen according to how you feel. If you are not currently exercising, take a daily walk. Start with 5 to 15 minutes a day. Adjust the distance and pace based on how you feel. The key thing is to find a balance between rest and activity.
Anemia, one cause of fatigue, may be treated with a medication called epoetin (Procrit, Epogen) or darbepoetin (Aranesp). This medication stimulates your bone marrow to make more red blood cells, raising your blood cell count and increasing your energy. It is given by injection under the skin using a very small thin needle. It comes in different doses and is commonly given once a week. You may be instructed to take an iron supplement by mouth while getting these injections. If you are anemic and feel fatigued, ask your doctor if this medication could help you.
If you have other specific problems that you think may be contributing to your fatigue, speak with your doctor or nurse about them. Ask them about taking a sleeping medication if you are having difficulty sleeping at night. Ask them about how to manage your pain better if you are not comfortable. Ask about how you can cope with emotional distress better. Ask them for advice on how to increase your food and fluid intake if you feel you are not eating and drinking enough.
Unfortunately, fatigue cannot always be effectively treated. It is often necessary to adjust your activity to accommodate to changes in your energy level.
Conserve your energy for the most important activities. Think about all the things you do during the day: working, shopping, cooking, cleaning, household chores, errands, taking care of children or dependent relatives, being with family and friends, and recreational or leisure activities.
Which of these activities are the most important? Which give you the most pleasure? Which make you feel good about yourself? Save your energy for them. You’ll probably notice that your energy is greater at certain times of the day. Plan your favorite activities for those times. For the other things that must get done, ask family and friends to help. People often want to be helpful but don’t know how. Tell them specifically what you need help with; they will probably be grateful for the direction.
Finally, let go of the things you don’t need to do and don’t want to do.
To learn more about fatigue, search on the following Internet sites:
• American Society of Clinical Oncology: www.cancer.net
• National Cancer Institute: www.cancer.gov
• American Cancer Society: www.cancer.org
Terms:
Myalgias - Aches and pains in the muscles.
Pruritus - A sensation that makes people want to scratch.
Jaundice - Yellowing of the skin and the whites of the eyes resulting from a buildup of bilirubin in the tissues; it can occur if the bile ducts are blocked or if the liver is not functioning, and is accompanied by a darkening of the urine and a lightening of stool color.
Anemia - A low red blood cell count. If you are being treated with radiation, contact your doctor or nurse before applying anything new to your skin to soothe irritation.
If you are being treated with radiation, contact your doctor or nurse before applying anything new to your skin to soothe irritation.
The key thing is to find a balance between rest and activity.
(12) Cancer Symptoms & Treatment
I have difficulty sleeping at night. What can I do to sleep better and feel more rested?
Difficulty sleeping is a common problem for many people-either with falling asleep in the evening or with staying asleep through the night. Aside from the distress of lying awake in bed for many hours, not getting enough sleep may cause you to feel irritable and tired during the day and to have difficulty concentrating. Try to determine whether there is a concrete reason you are not sleeping. Are you physically uncomfortable or in pain? Are you having other symptoms, like nausea, vomiting, diarrhea, constipation, itching, mouth sores, or anything else that is preventing sleep? Take medication, as prescribed, to get a restful night’s sleep. If you are taking medication and it is not effective, tell your doctor or nurse.
Aside from physical reasons for not sleeping, are you feeling anxious and worried at night? Are your thoughts racing and keeping you awake at night?
Speak with someone you trust, someone supportive, about your thoughts and feelings; this may provide a significant amount of relief. For some people, medication for anxiety may be helpful.
Do you feel generally restless at night, unable to relax and sleep? A variety of techniques may help:
• Establish a regular schedule, going to bed and waking up at the same times every day.
• Even if you do not sleep well at night, try not to sleep excessively during the day. Naps disrupt your body’s normal cycle. If you are very tired, take a short nap during the day, but not for more than an hour.
• Avoid being in bed at any time except when you are going to sleep. When resting during the day, lay in another room, on a couch or chair. Use your bed only for sleep at night.
• Avoid drinking caffeine or stimulants after dinner.
For some people, these techniques aren’t helpful. If you continue to have difficulty with sleep, ask your doctor to prescribe a sleeping medication. Getting a restful sleep at night is important to feeling energized and capable during the day.
Is there medication I can take to treat my fatigue?
One cause of fatigue is anemia, a low red blood cell count. Red blood cells are produced in the bone marrow and released into the bloodstream, where they carry oxygen from the lungs to all the tissues of the body. The cells use the oxygen to create energy. When the red blood cell count is low, less oxygen is available to the cells, resulting in fatigue. The number of cells in the blood can be measured by testing a blood sample for what is called a complete blood count (CBC). The number of red cells is also reflected in measurements called hematocrit (the percentage of red cells in the blood) and hemoglobin (the substance in red blood cells that binds to oxygen and carries it to the tissues of the body). The normal ranges for these tests vary from laboratory to laboratory, but in general they are as follows:
• Hemoglobin: 12–18 grams per deciliter (g/dl)
• Hematocrit: 36–54%
Of the many causes of fatigue, if the cause is anemia, your doctor will need to determine the reason for it and decide how to treat it. If you are undergoing chemotherapy and your hemoglobin is lower than 10 g/dl, treatment with a medication called epoetin (Procrit, Epogen) or darbepoetin (Aranesp) may be helpful. This medication stimulates your bone marrow to make more red blood cells, raising your blood cell count, delivering more oxygen to the body, and increasing your energy. It is given by injection under the skin using a very small thin needle. It comes in different doses and is commonly given once a week.
Your doctor may also decide to treat your anemia with a blood transfusion. Both treatments have their risks and benefits, and you and your doctor will decide which is best for you. Along with either treatment, you may also be instructed to take an iron supplement. You can obtain additional information about the use of epoetin and darbepoetin on the Internet (www.cancer. net).
Can I exercise?
Pete’s comment:
Exercise has been an integral part of my life for the last 20 years, and I was concerned that my cancer treatment might cause me to cut back. I was encouraged by my oncology team to ease back into an exercise regimen as quickly as possible. I started with chair aerobics and one-on-one personal training with a clinical nurse specialist. I was eventually able to get back to a full workout routine at my gym, which has given me both a mental and physical lift.
The benefits of exercise are well-known. The American Cancer Society and other organizations recommend exercise for promoting health and for the prevention of many diseases (e.g., heart disease, high blood pressure, cancer). Many studies have shown that exercise may play a role in the prevention of breast, prostate, and colon cancers. Some people believe that they should “conserve their energy” during the diagnosis, treatment, and recovery phases of cancer. However, having a diagnosis of cancer does not mean you have to stop exercising. Studies have shown that people with cancer enjoy many benefits from exercise, including:
• Reduced feelings of anxiety, stress, and depression
• Decreased treatment-related side effects (nausea, constipation, and fatigue)
• Improved appetite and sleep
• Improved bone strength and muscular flexibility
• Improved quality of life and feelings of general well-being
Here are some general guidelines about exercise:
• Before you start or resume exercising, check with your doctor or nurse to see whether you should avoid some types of activity.
• Most people have no limitations on exercise. If exercise was a part of your routine before cancer diagnosis, you should be able to keep up the same routine during diagnosis and treatment.
• After some types of surgery (breast surgery, lung surgery), your doctor or nurse will recommend therapeutic exercises.
• Exercise should not cause pain or discomfort. You should participate in enjoyable activities.
If you have been in bed or have not exercised in a long time, performing everyday activities yourself is a good way to get started. Adding exercise to your daily routine can be as simple as taking a walk outside to get the paper or mail, doing light housekeeping, or shopping for food. In general, it is important to start slowly and increase your exercise level gradually.
Others may enjoy yoga or other structured exercise classes offered at fitness centers. Exercise and yoga videotapes are also available at public libraries for those who want to work out at home. Some people participate in aerobic exercise and weight-training activities. Studies have shown that structured exercise programs helped cancer patients improve endurance, strength, and flexibility, and these patients return to everyday activity faster than those who do not exercise. There may be specific exercise groups in your area for cancer survivors or those who are actively undergoing cancer treatment. Some hospitals and universities have wellness programs (including nutrition and exercise) for people with cancer. Local fitness centers (e.g., the YMCA) may also provide classes for those undergoing cancer treatments.
Terms:
Hematocrit - The percentage of red cells in the blood.
Hemoglobin - The substance in red blood cells that binds to oxygen and carries it to the tissues of the body.
Try to determine whether there is a concrete reason you are not sleeping.
People with cancer enjoy many benefits from exercise.
If exercise was a part of your routine before cancer diagnosis, you should be able to keep up the same routine during diagnosis and treatment.
(13) Cancer Symptoms & Treatment
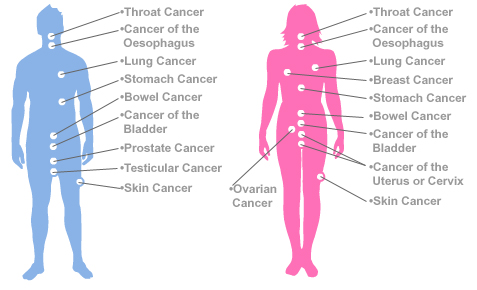
Signs and Symptoms of Cancer - American Cancer Society
15 Cancer Symptoms Women Shouldn't Ignore

BLOOD COUNTS AND YOUR IMMUNE SYSTEM
I have heard that chemotherapy may cause drops in my blood counts. What does this mean?
Bone marrow produces blood cells and releases them into the bloodstream, where they are able to protect the body in a variety of ways.
• White blood cells are cells in the blood that fight off infection and other types of disease; there are many different types of white blood cells, including neutrophils and lymphocytes.
• If you are cut or injured, platelets, also called thrombocytes, are blood cells that stop bleeding by clumping together, or clotting, to plug up damaged blood vessels.
• Red blood cells, also called erythrocytes, are cells in the blood that contain hemoglobin that carries oxygen from the lungs to all the tissues in the body; the cells use the oxygen to create energy. The number of cells in the blood can be measured by testing a blood sample for a complete blood count (CBC). The number of red cells is also reflected in measurements called hematocrit (the percentage of red cells in the blood) and hemoglobin (the amount of the molecule carrying the oxygen in the red cells).
The normal ranges for a CBC vary from laboratory to laboratory, but in general the normal values are as follows:
• White blood cells: 4-10,000 cells per cubic millimeter (cells/mm3)
• Platelets: 150,000–500,000 cells/mm3
• Hemoglobin: 12–18 g/dl
• Hematocrit: 36–54%
Once the bone marrow releases the blood cells into the bloodstream, they live for only a short time: as short as 24 hours for some types of white cells, about 10 days for platelets, and about 3 months for red cells. The body depends on the rapidly dividing cells in the bone marrow to continuously replace these cells as they die.
Chemotherapy destroys tumor cells by preventing them from dividing. However, normal cells that divide rapidly, such as those in the bone marrow, are also very sensitive to chemotherapy. The bone marrow loses the ability to form new blood cells; so fewer cells are released into the bloodstream, and the blood counts drop, generally 7 to 14 days after a chemotherapy treatment.
The white cells and platelets are particularly sensitive because they live only a short period of time. The body can adjust to slight decreases in the number of blood cells without any problem; however, your doctor will order a CBC before you get each cycle of chemotherapy to be sure that your counts are not too low. If your white cell or platelet count is too low, your doctor may decide to hold your treatment for a week to give the bone marrow a chance to make new blood cells.
Radiation therapy may also cause a drop in your blood cell counts if it is directed to an area that contains a large amount of active bone marrow, such as the pelvis, the ribs, or the spinal column. If there is a chance that your blood cell counts will drop during treatment, your doctor will order a CBC every week or two during your treatment.
What do I do if my white blood cell count is low?
If your white blood cell (WBC) count drops, the question is which types of white blood cells are low? The doctor will order a CBC that lists the different types of white blood cells found and the number of each.
Neutrophils, a type of white blood cell that fights bacterial infection and other diseases, make up about 45-75% of your white blood cells. If the count is low, you have an increased risk of developing an infection.
Throughout your treatment, you can do certain things to prevent infection:
• Wash your hands frequently with soap and water, especially before eating and after going to the bathroom.
• Bathe daily with soap and water, and brush your teeth after each meal.
• Avoid people with colds or flu.
• Avoid sharing food utensils, drinking glasses, or toothbrushes.
• Avoid handling pet feces or urine, especially in cat litter or birdcage droppings.
• Check with your doctor or nurse before having any dental work or immunizations.
You can develop neutropenia, a decrease in the number of neutrophils, the type of white blood cell that fights bacterial infection and other diseases. In that event, your doctor or nurse may advise you to take extra precautions to prevent infection. In addition, your doctor may prescribe a medication called filgrastim (Neupogen®) or pegfilgrastim (Neulasta®) that can stimulate the bone marrow to make new white cells quickly. It is injected under your skin with a small thin needle. You or a family member may be taught to give the injection at home.
Despite doing all the right things, you may still develop an infection. If you have any implanted catheters or tubes (such as a port, a urinary stent, or a biliary stent) you have a higher than normal risk of developing an infection. You will not feel that your WBC count is low, so call your doctor or nurse if you develop any signs or symptoms of infection. You will most likely need to be examined and have tests taken to determine whether you require treatment with antibiotics.
Reasons to call the doctor:
• Fever of 100.5ºF (38ºC) or higher
• Shaking chills
• Sore throat or cough
• Frequency or burning when you urinate
• Swelling, redness, or pain anywhere on your skin
• Vomiting or diarrhea unrelated to your chemotherapy
To learn more about neutropenia and how to manage it, search on the following Internet sites:
• Oncology Nursing Society: www.cancersymptoms.org
• American Society of Clinical Oncology: www.cancer.net
• National Cancer Institute: www.cancer.gov
• American Cancer Society: www.cancer.org
What do I do if my platelet count is low?
If your platelet count drops, there is an increased risk of bleeding. Throughout your treatment, unless prescribed by your doctor, avoid aspirin, products that contain aspirin, and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, because these may all interfere with platelet functioning. If the platelet count drops very low, your doctor or nurse may advise you to take extra precautions to prevent bleeding, such as using only an electric razor and avoiding activities in which you could be injured.
You will not feel that your platelet count is low; so call your doctor or nurse if you develop any signs or symptoms of bleeding.
Reasons to call the doctor:
• Easy bruising
• Bleeding gums or nosebleeds
• Blood in the urine or stool
• Black stools
What do I do if my red blood cell count is low?
If the red blood cell (RBC) count drops, you will feel fatigued. Fatigue can be experienced in many different ways: lacking energy; feeling tired, weak, or weary; feeling irritable or depressed; or having difficulty concentrating.
You may even feel lightheaded or short of breath. If the RBC count falls very low, your doctor may recommend a medication called epoetin (Procrit®, Epogen®) or darbepoetin (Aranesp®), which stimulates the bone marrow to make more red blood cells. It is given by injection under the skin using a very small thin needle. It comes in different doses and can be given either three times a week or once every 1 to 2 weeks.
Some people give themselves the injection; some people get it from their oncology nurse. You may also be instructed to take an iron supplement by mouth while getting these injections.
To learn more about anemia and how to manage fatigue, search on the following Internet sites:
• Oncology Nursing Society: www.cancersymptoms.org
• American Society of Clinical Oncology: www.cancer.net
• National Cancer Institute: www.cancer.gov
• American Cancer Society: www.cancer.org
Terms:
White blood cells - Cells in the blood that fight off infection and other types of disease; there are many different types of white blood cells, including neutrophils and lymphocytes; also called leukocytes.
Platelets - Cells in the blood that stop bleeding by clumping together, or clotting, to plug up damaged blood vessels; also called thrombocytes.
Red blood cells - Cells in the blood that contain hemoglobin that carries oxygen from the
lungs to all the tissues in the body, which the cells use to create energy; also called erythrocytes
Neutrophils - A type of white blood cell that fights infection and other diseases.
Neutropenia - A decrease in the number of neutrophils, the type of white blood cell that fights bacterial infection and other diseases.
Your doctor or nurse may advise you to take extra precautions to prevent infection.
If your platelet count drops, there is an increased risk of bleeding.
(14) Cancer Symptoms & Treatment
Side Effects of Radiation Therapy

CARING FOR YOUR SKIN AND HAIR
I have heard that radiation therapy causes a skin reaction. Is this true? How should I care for my skin during radiation therapy?
Radiation therapy is administered as a beam of energy directed from a treatment machine at precise angles toward a defined target in your body. It destroys tumor cells in its path by preventing them from dividing. Normal cells that divide rapidly are also very sensitive to radiation therapy. As a result, there may be changes in your skin where the beam enters and exits your body. After about 2 weeks, you may notice redness, tanning, dryness, flaking, and/or itching. If you are being treated in sensitive areas of the body, such as the armpit, the neck, under the breasts, and the perineum (the area between the genitals and the anus), the reactions may become more severe over time, and you may develop blistering and weeping of the skin. Ask your doctor or nurse to explain what you should expect based on the area being treated. These effects are all expected, and they will heal about a month after treatment is completed; however, you may be left with an area of darkened skin in the treated area.
Take special care of your skin from the first day of treatment to ensure that you do not become uncomfortable from any changes. Bathe daily using warm water and a mild, unscented soap, such as Dove, Neutrogena, Basis, or Cetaphil. Do not scrub the skin with a cloth or brush, rinse the skin well to get off all the soap, and gently pat it dry. Your doctor or nurse may recommend the use of a moisturizer, either from the beginning of treatment or if you develop dryness or itching. Examples of products often used during radiation therapy are Aquaphor, Eucerin, Biafine Topical Emulsion, and products with aloe vera gel, calendula, or hyaluronic acid.
There is no compelling evidence that any one product is better than the other. Ask your doctor or nurse for a recommendation on application. The common recommendation is to use the moisturizer twice a day, after your daily treatment and at bedtime. Check before using any other lotions, creams, or ointments in the area being treated because some products can make the skin reaction more severe.
Avoid irritating the skin. Follow these suggestions in the area being treated:
• Avoid tight, constricting clothing.
• If treatment is to the pelvis, wear cotton underwear.
• Avoid the use of tape.
• Avoid scratching the skin. Tell your doctor or nurse if the moisturizers are not effective in relieving the itching so that something else can be prescribed.
• Avoid direct sunlight.
• Avoid the use of ice packs or heating pads.
Radiation therapy will also cause the hair in the treated area to fall out. If you are not being treated in the head or neck area, you will not lose any hair on your head. Your hair will grow back several months after your treatment is completed.
I have heard that chemotherapy may cause me to lose my hair. Can I prevent this? What can I do to feel good about my appearance if I lose my hair?
Chemotherapy destroys tumor cells by preventing them from dividing, and normal cells that divide rapidly are also very sensitive to chemotherapy. The cells at the base of the hair follicle may become unable to divide to make new cells, weakening the hair shaft and resulting in hair loss. Some people experience only a thinning of their hair, but others lose all the hair on their head.
Certain chemotherapy drugs are much more likely than others to cause hair loss. Your doctor or nurse can tell you if you are likely to lose your hair based on the type of chemotherapy drug that you are receiving. If you are receiving chemotherapy drugs that are likely to cause hair loss, you might lose hair from other parts of your body. Hair anywhere on your body can be affected, including your eyebrows, eyelashes, and hair in your underarm and pubic areas. Hair loss usually begins about 3 weeks after chemotherapy begins. Sometimes people notice a gradual thinning and loss of hair, but with some chemotherapy agents the hair can come out in clumps over a period of only a few days.
If you are receiving chemotherapy that causes only a thinning of hair, you can reduce the amount of hair you lose:
• Use a mild shampoo, such as baby shampoo.
• Use a soft-bristled hairbrush.
• Avoid permanents and hair dyes.
• Avoid heated rollers and high-heat hair dryers.
If you are receiving chemotherapy with a high likelihood of causing complete hair loss, there is no way of preventing this. Doctors no longer use ice caps to prevent the chemotherapy from flowing to the scalp because they want to be sure the chemotherapy travels all over your body, not missing any area where there could be cancer cells.
If you are likely to lose your hair from treatment, you may find it helpful to purchase a wig or hairpiece beforehand. Some people like to match their own hairstyle to maintain their usual appearance; others like to try a new look. Wigs can be made with human hair or from synthetic fibers, and they vary considerably in price. Look for stores in your area that specialize in working with people who lose their hair from cancer treatment or you can purchase a wig or hairpiece through the American Cancer Society. Your local American Cancer Society or hospital social work department may also have wigs and hairpieces available on loan. Your insurance company may cover the cost of the hairpiece. Check your policy, and, if it is covered, ask your doctor to write you a prescription for a “hair prosthesis needed for cancer treatment.”
Costs that are not reimbursed are tax deductible. Some people prefer to wear a turban, scarf, or cap to cover their heads, and some prefer to leave their head uncovered. Do whatever makes you feel the most comfortable. The important thing is not to let your changed appearance alter your willingness to interact with family, friends, and coworkers.
Despite the loss of hair, you can take many steps to feel good about your appearance: for example, taking care of the clothes you wear, using makeup if you like, and wearing scarves or caps. The Personal Care Products Council, the National Cosmetology Association, and the American Cancer Society sponsor a free program, “Look Good, Feel Better,” that is dedicated to helping men and women being treated for cancer feel better about their appearance. The program offers beauty techniques that help restore your appearance and enhances your self-image, provides many tips on its Internet site, and presents group programs all over the country. To find out if the program is available in your area, check their Internet site (www.lookgoodfeelbetter.org).
I have heard there may be changes in the color of my skin from my treatment. What does this mean?
Color changes in skin and nails can occur during treatment for cancer. These color changes are usually temporary and can be caused by either chemotherapy or radiation therapy.
Changes in skin and nails include:
• Flushing
• Hyperpigmentation
• Photosensitivity
Flushing is a temporary redness that usually occurs in the face and neck as a result of dilated capillaries, which are small blood vessels located just under the surface of the skin. Flushing can be caused by chemotherapy (paclitaxel, cisplatin, doxorubicin), intravenous contrast (used with CTs), or some oral medications (steroid medicines such as prednisone or dexamethasone). Sometimes flushing is accompanied by a feeling of warmth. Flushing is always temporary and generally lasts for minutes or up to several hours.
Call your doctor or nurse if the flushing is persistent or accompanied by pain, fever (100.5ºF or more), swelling, or another discomfort.
Hyperpigmentation is a darkening of the skin, such as a freckle. This darkening can be generalized, as in a suntan, or localized to certain areas of the body. If localized, you may notice darkening of the skin over finger joints or elbows and knees. The palms of the hands and soles of the feet may also darken, as may the tissue under the fingernails and toenails or the nails themselves. There may even be color changes in your mouth, for example, darkening of your tongue and gums. Certain intravenous chemotherapy (fluorouracil) causes darkening along the length of the vein into which it is given. Hyperpigmentation may be more noticeable in people with darker skin tones. Some types of chemotherapy (paclitaxel or docetaxel) cause white lines, called Beau’s lines, to form horizontally on the fingernails. Radiation therapy can cause the skin to darken in the irradiated area. Sun exposure may increase hyperpigmentation temporarily. Hyperpigmentation usually occurs within several days to 2 to 3 weeks after starting treatment. Sometimes the discoloration is permanent, but usually, it resolves within a few months after treatment is completed.
Photosensitivity means that your skin is more sensitive to the sun (i.e., ultraviolet radiation); you can burn more easily when in the sun or you may develop a rash from it. This reaction can occur whether you have light or dark skin, and it may result from medications, including certain types of chemotherapy and antibiotics.
Radiation therapy can also cause the skin in the treated area to be more sensitive to the sun. Before going out in the sun, ask your doctor or nurse if you are taking any medications that can cause this reaction. Photosensitivity can result in severe sunburn, but this reaction can be prevented. When outside, even on cloudy days, wear protective clothing, including a hat, long-sleeved shirt, and long pants, and always use a sunscreen with an SPF of at least 15. At the beach, sit under an umbrella and use a sun block such as zinc oxide.
If you get a bad sunburn or rash from the sun, call your doctor or nurse. They can prescribe medicines to make you more comfortable. They can also tell you which lotions or creams are best to use for the sunburn.
Lisa’s comment:
I’m a beach bum-love the summer, love the beach, love the ocean. I have a cabana at Malibu Beach (Long Beach, Long Island). Photosensitivity was probably one of the biggest obstacles for me. I had to wear sunscreen (well, that wasn’t new), sit under an umbrella, and not go in the ocean (that wasn’t because of chemotherapy, but because of surgery restrictions). I felt like my one true pleasure was a chore, a burden. I did very well with keeping myself protected from the sun, but I really didn’t entirely enjoy my days at the beach. But, chemotherapy didn’t stop me from going! My fingernails turned a yellowish-orange color with the adriamycin/Cytoxan therapy.
Take special care of your skin from the first day of treatment.
Certain chemotherapy drugs are much more likely than others to cause hair loss.
Do whatever makes you feel most comfortable
Skin and nail color changes are usually temporary.
(15) Cancer Symptoms & Treatment
How Is Chemotherapy Used to Treat Cancer?

CARING FOR YOUR SKIN AND HAIR
I have heard that some chemotherapy drugs can burn your skin.What does this mean?
Most chemotherapy drugs are given through a vein, and oncology nurses are specially trained to administer these drugs safely and accurately. Despite using the most careful technique, the drugs can sometimes leak out of the veins into the surrounding tissue and collect under the skin (extravasation). In these cases, the vein is said to be “blown.” The body reabsorbs most chemotherapy fluids with no ill effects. However, some chemotherapy drugs, call vesicants, can cause blistering or other local tissue damage if they leak from a vein into the surrounding tissue. Examples are cisplatin, doxorubicin, vincristine, and paclitaxel. Other chemotherapy drugs may cause irritation and inflammation if they leak under the skin but will not cause any tissue damage.
If you feel pain or burning while your nurse is giving you treatment, say so right away. If there is any indication that chemotherapy has leaked out of the vein, the nurse will stop the treatment and remove the needle. If the chemotherapy is a vesicant, the nurse may apply hot or cold compresses or inject or apply special medicine to the area. Keep an eye on the site over the next 2 weeks. Very rarely, serious reactions can develop. Call your doctor or nurse if you have pain, if the area becomes red or swollen, or if you see blisters or ulcers. The doctor will reevaluate you and refer you to a plastic surgeon if necessary.
Lisa’s comment:
I wanted a mediport as soon as I heard I would need chemotherapy. I had always told my patients, “If I were to get chemo, I would get a mediport.” I said it because I meant it. Being diagnosed with breast cancer and requiring an axillary node dissection meant I only had one arm available for intravenous therapy. I knew I was scheduled to receive adriamycin/paclitaxel-vesicants. So, I really wanted a mediport. I guess deep down I didn’t trust anyone to give me chemotherapy. Needless to say, the Breast Service didn’t recommend port placement for only eight cycles of chemotherapy-not worth the surgical risks. I did fine. The nurses did not have trouble with my veins, and I never had an extravasation.
What is jaundice and how can it be treated?
When the liver breaks down haemoglobin, the oxygen-carrying substance in red blood cells, it produces bilirubin, which is then incorporated into the bile, giving it a yellow-green colour. Bile is stored in the gallbladder. After someone eats, the gallbladder pushes the bile out through the bile duct into the intestine where it digests certain types of food. The bile is then eliminated in the stool, and the bilirubin helps to give stool its usual brown colour.
If bilirubin builds up in the bloodstream, it lodges in the skin and eyes, causing them to become yellow. This condition is referred to as jaundice (or icterus). Some of this excess bilirubin, as it is eliminated in the urine, darkens the urine. If the bilirubin is not able to pass into the intestine, the stools become lighter in colour. People with cancer may develop increased bilirubin and jaundice for a number of reasons. The body is either not eliminating enough bilirubin or producing too much of it. A mass in the bile duct or in the area around the duct (e.g., in the gallbladder, liver, or pancreas) may block the flow of bile though the duct, interfering with elimination. Disease in the liver may also reduce the body’s ability to eliminate bilirubin. Certain blood disorders in which a large number of red blood cells are destroyed may cause increased levels of bilirubin. Sometimes jaundice can be treated. If the bile duct is locally blocked, a small hollow tube can be inserted to open the duct by relieving the obstruction. If the liver disease or blood disorder is treatable, the bilirubin level will come down. However, if jaundice cannot be treated, there are ways to ensure that you are comfortable. Jaundice itself causes no pain, but the skin may become very dry and itchy. Scratching may create breaks in the skin, which could become infected; so preventing itching is important. Treating the dryness eases the itching. When bathing, avoid very hot water and use only mild soaps. Apply skin lotions or creams after bathing and throughout the day as needed to moisturise the skin. If you still feel itchy, ask your doctor for a prescription for medication to reduce the itching.
What do I do if I get a rash?
A rash is a skin reaction that may be localised to one area of the body or that may cover most or all of the body (generalised ). Rashes may cause itching or pain. Medicine is the most common cause of rashes, which can be a side effect of the medicine (e.g., causing an acne-like rash) or a sign of an allergic reaction. An illness caused by a virus, such as measles or shingles, can also cause rashes. Other causes are changes in laundry detergent, moisturiser, or soap. If you develop a rash, call your doctor or nurse.
Be prepared to tell:
• Where the rash is located
• What the rash looks like
• When it started
• Whether you have any other symptoms, such as fever, itching, or pain
• If you have recently started using a new medicine
Words that can be used to describe a rash are raised (bumpy), flat, or blistered. Describe the colour, for example, as red, purplish, or skin colour. If the rash is an expected side effect of the chemotherapy you are taking, your doctor or nurse will advise you on what products are best to use on your skin. If itching is associated with the rash, your doctor may prescribe an antihistamine, a medication that is used to prevent or treat allergic reactions and that is sometimes given to treat itching caused by a rash. Diphenhydramine is an antihistamine that can be bought over the counter. An antihistamine may make you sleepy and give you a dry mouth. For an itchy rash, your doctor may also prescribe calamine lotion and/or take a bath with Aveeno or oatmeal. If your rash seems to be from an allergic reaction to your medicine, the doctor may tell you to stop taking it. If your rash is from shingles, the physician will prescribe an antiviral medicine.
If you also have hives or difficulty breathing, call your doctor and go to the nearest emergency room.
Mary Ann’s comment:
If you get a rash, call your doctor. There are excellent creams and powders to aid in the relief of rashes. When I first began my program, I had terrible rashes beneath my breasts, in any “fat roll” on my stomach, and in a rather not-talk-about place. Antifungal medication resolved the problem within a few days. There is no reason to be uncomfortable. Speak up!
Terms:
Extravasation - A potential complication of intravenous chemotherapy administration that occurs when chemotherapy leaks from the vein into the surrounding tissue.
Vesicant - A type of chemotherapy that causes blistering or other local tissue damage if it leaks from a vein into the surrounding tissue.
Antihistamine - Medication that is used to prevent or treat allergic reactions and that is sometimes given to treat itching caused by a rash
If you feel pain or burning while your nurse is giving you treatment, say so right aw



































