General Cancer
COURSE
Understanding and Prevent Cancer
(68) General Cancer

Radiation Therapy
Radiation therapy (RT) brings waves of energy particles into contact with cancer cells. It can be delivered by an external beam through a machine called a linear accelerator (the most common form of RT), directly implanted into a cancer in the form of radioactive seeds (called brachytherapy), administered intravenously (such as radioactive iodine given for thyroid cancer), or coupled to monoclonal antibodies (such as Bexxar and Zevalin used to treat lymphoma). RT is also used in other ways.
It is tempting to think of radiation therapy as zapping cancer cells much like a laser in Star Wars obliterates an enemy ship. In fact, though, patients receiving RT are told that an MRI or CT scan to assess the results of their treatment will not be performed for several weeks after the completion of RT in order to “give the treatment time to exert its full effect.” This is because radiation delivers an energy burst to cells, setting in motion a number of reactions that over time cause the cell to die. Just like the drug therapies discussed above, radiation can cause damage to DNA and interference with the signals communicated inside cancer cells; it can even exert an angiogenesis inhibitory effect by killing the endothelial cells that form blood vessels. The result is that RT causes cancer cells to undergo cell death.
To improve the results with radiation, researchers are studying the addition of targeted therapies to RT. One of the most impressive results was recently reported using Erbitux in combination with RT to treat head and neck cancer. The combination greatly increased survival compared to treatment with radiation alone. The addition of chemotherapy to this combination is being studied.
Why Do Cancer Treatments Sometimes Fail?
Drug resistance or the growth of cancer in the face of ongoing or recently completed treatments represents the main barrier to cure for many cancers. When a patient experiences a remission, his or her hopes for cure or prolonged cancer control are naturally raised. It is therefore upsetting and often disorienting to be told that the cancer has relapsed, that the treatments have suddenly stopped working.
In most instances, oncologists cannot specify why a person’s cancer develops treatment resistance. We rely on the discoveries of laboratory researchers, who themselves are busy sorting through the myriad of possible scientific reasons for resistance to just one particular drug. If this seems like a bit of double talk, it just might be; treatment resistance is probably the most complicated area of oncology. The root cause of a cancer relapse lies in the fact that cancer is not an accumulation of exactly the same cells but rather a mixture of cells with differing properties. Some may have sensitivity to certain drugs and be killed by them, whereas others are resistant to those drugs. The resistant population will survive treatment and in time be detected as a cancer relapse. For cancers that can be cured, the available therapies can match all that the cancer can offer by way of resistance. For those that cannot be eradicated, newer treatments are needed that overcome this resistance.
Drug resistance may be present in an untreated cancer or emerge in response to therapy. This property explains the acquisition of resistance during a cancer’s growth.
Chemotherapy may lose its effectiveness when cancer cells activate a protein that pumps the drugs out as soon as they enter the cells; targeted therapies may lose their ability to control their targets when those receptors and signaling proteins mutate and morph into different shapes; hormone therapies may stop controlling cancer growth when the estrogen or androgen receptors undergo a shape change or get massively overproduced, overwhelming the drugs meant to neutralize them. Through an understanding of the specific genes and proteins responsible for drug resistance, researchers are developing new chemotherapies, targeted therapies, and hormone treatments that may be effective when available treatments stop working.
Exciting new research is shedding light on the “natural” drug resistance of some cancers. Several types of cancer have been found to contain a very small population of cancer stem cells, which are believed to be responsible for continually replenishing the pool of cells in a tumor.
It turns out that an additional property of these cancer stem cells is their natural resistance to chemotherapy and other cancer treatments.
If the molecules driving the growth of these cells could be specifically targeted by drugs, the treatment of many cancers may improve. The first reported payoff of this approach was presented at the 2008 meeting of the American Association for Cancer Research (www.aacr.org). The study involved patients with aggressive basal cell skin cancer treated with a pill (named GDC-0449) that targets a molecule called “hedgehog.” Of the first nine patients enrolled in the study, eight experienced shrinkage or no further growth of their cancer. Targeting cancer stem cells will undoubtedly be an important avenue of research in the years to come.
Breast and prostate cancers depend on the hormones estrogen and testosterone to make them grow. Hormone therapies decrease the levels of hormones, resulting in cancer death.
(69) General Cancer

Get Prepared to Survive
At our cancer center we have a ritual to celebrate the completion of each of our patients’ cancer treatments. When the last chemotherapy bag has run dry, the oncology nurse escorts him or her to a bell located at the entrance of the infusion suite.
An announcement goes forth: “They’re going to ring the bell!” There is a flurry of happy scurrying as staff members rush to join family and friends to witness the momentous occasion. If it’s a woman, she may don a diamond tiara (the ninety-nine-cent kind); if it’s a man, he’ll probably skip that part of the commemoration (or wear it for fun). The patient rings the bell amid a swirl of smiles, cheers, and sincere good feelings. The release feels great. Perhaps this moment was six months or a year in the waiting. Patients sometimes ring that bell again for emphasis and then hug those whose love and support saw them through; they may shout, raise their arms in victory, cry, or just exclaim, “I’m outta here!” As the patient leaves the center, however, the familiar path is somehow different. This time the exit leads not just to the outside but to the future-a future that is full of hope but also full of uncertainty. The transition from the end of treatment to the rest of one’s life presents many challenges. Few people can merely “pick up where they left off” the life that they knew before they had to confront cancer. For most, cancer changes everything. In the past, cancer patients received little guidance about coping in the aftermath of treatment or what to expect from follow-up care. Many survivors felt abandoned once the intensive therapy and checkups ended. All this is changing. In 2005 the Institute of Medicine, an expert health care advisory panel, issued From Cancer Patient to Cancer Survivor: Lost in Transition. This report outlines the many needs of survivors and directions for health care professionals to address them. It recommends that each person completing cancer treatment be counseled and given a treatment plan and summary (called a Survivorship Care Plan) outlining their follow-up care. This plan is to be shared with the patient’s primary care doctors to help coordinate care among providers. For patients living with cancer who require ongoing therapy, a modified plan is issued from time to time or when treatment regimens change. The typical care plan contains the following elements:
1. A summary of the patient’s diagnosis and treatment history
2. The potential long-term effects from therapy
3. Recommended cancer surveillance (tests and schedules)
4. Healthy living goals
5. Further discussion of family history and need for genetic testing
6. Reassessment of the patient’s emotional (psychological) needs and information on the community resources available to address them
7. Reassessment of the patient’s practical needs, such as those related to employment and health insurance, and information on resources to address them
I want you to know that the doctors, nurses, social workers, patient advocates, and all those who work with cancer patients understand that almost every patient will face some new psychological, social, and/or physical issue as a result of having to deal with this disease. Many dedicated professionals, volunteers, and organizations are available to assist survivors in dealing with cancer and its many ramifications on their lives. Sadly, many survivors do not find the help they need, either because they don’t feel they need it or their physicians do not make the necessary referrals.
For example, regarding psychological or emotional counseling, I have heard many patients and family members’ state, “I wish I had gone for counseling, but I didn’t.”
It is crucial that all people who are affected by cancer, no matter how strong they may think they are, seek out the appropriate help that will make their long-term recovery as full and vigorous as possible.
Survivorship and the Power of People
From the moment a person is diagnosed with cancer through all of the treatments and then for the rest of his or her life, that person is considered a cancer survivor. The “process” of surviving cancer is called survivorship, and it is indeed a process.
I am not a cancer survivor. Neither am I a counselor or therapist. Yet I have intimately witnessed the effects of this disease on beloved family members and friends. And I have cared for and learned from many people who have fought hard against cancer. Each has his or her own needs and each will handle the ordeal in his or her own way. I and all those who participate in caring for people with cancer are humbled and renewed every day by bearing witness to the tremendous power of the human spirit and the unbelievable generosity of the human heart. I have seen people rise above great adversity, marshal their physical strength and mental toughness, and smile. I have seen women lose beautiful hair (and more of course) and laugh. I have seen vigorous men made weak but still smile and in time regain their vitality. And when the fight against cancer cannot be won, I have seen people die with tremendous dignity, doing it their way, surrounded by love. I have seen their friends and family turn grief into generous acts of volunteering and fund-raising. I have seen people meet these challenges because life is our most precious gift, worth fighting for and worth remembering. As Max Ehrmann wrote in the poem “Desiderata,” “With all its sham, drudgery and broken dreams, / it is still a beautiful world.” Cancer may challenge us, but it cannot destroy our spirit and who we are. This I have learned. I have also come to learn of a special force, which I now call “the power of people.” Although our religious beliefs may differ, one mystical occurrence that I am certain exists for us all is the power of people. When a volunteer gives a cancer patient a cup of coffee and a smile, when one patient calms the fears of another, when women with cancer get together to put on makeup, when a patient says to me, “I am praying for you and your family,” when a boss tells an employee battling cancer, “Take as much time as you need, your job will be here for you,” when a nurse makes a home visit to a patient in the middle of the night to alleviate pain, when the local fire department sends a truck and firefighters to celebrate the birthday of a young boy whose mother is battling cancer, when neighbors drop off meals for months on end to a family in need, when entire religious congregations pray for the health of someone they may not even know, when a thousand cancer survivors walk to celebrate life, everyone is lifted up. The power of people: magical, mystical, real. If you have cancer and feel like withdrawing into a shell, you can do that for a time. Then reach out and make the human connections that will help you heal
(70) General Cancer
Animated Introduction to Cancer Biology
PATTERNING YOUR LIFE AS A SURVIVOR
Survival is all about living, how you live day to day despite cancer. I introduced the term “pattern for living” to describe each individual’s daily habits and thought patterns. Once cancer strikes, one’s pattern for living is absolutely altered by virtue of having to deal with the psychological and physical impact of the diagnosis. Yet cancer brings to the fore a powerful life force that makes one want to live more than ever. For some, maintaining as much normality as possible is the optimal way to savor life. Others, however, may feel sufficiently shaken by the diagnosis to want to make changes in their lives.
But will these changes be only temporary? What about after the initial period of shock and later acceptance of the diagnosis? What about after treatment ends, or if treatments continue off and on for years? Can the same patterns for living that held sway before cancer continue afterward?
These are the critical questions that each survivor will have to ask him or herself. Certainly, cancer causes fear for one’s health and life, for one’s very being. But for most people, life will go on after cancer is diagnosed, and so I suggest that each survivor ask him or herself, “Do I need to make any changes to my life? Can I use cancer as a turning point?” Cancer can provide the pause you need to look at how you take care of your body, deal with the stresses of life, and cope with emotional challenges that may have been simmering for years. Did you worry excessively about your life before cancer? Are there personal relationships that need attention and repair? Does your job fulfill you to the extent it should?
When you hear people say things like “Cancer made me a better person” or “Cancer was the best thing that ever happened to me,” instead of thinking that these people are half-baked, realize that what they mean is that they used the challenge of cancer to jar their life into a better place. You can, too. Use the positive forces around you along with your own inner strength to change a dysfunctional pattern of living, to make good choices for your life. You will feel better for it and have more peace of mind to cope with cancer as a result. As a cancer survivor, you will face many challenges. Two of the most important types are physical and psychological (emotional).
PHYSICAL CHALLENGES
The physical challenges facing survivors fall into two main categories:
(1) recovery from the side effects of treatment; and (2) monitoring the body for a cancer recurrence or new cancer.
Recovery from treatment. The first aspect of recovery from the physical side effects of cancer treatment involves improving your general health. It is important to recognize that you may need to change your lifestyle. In the book After Cancer Treatment: Heal Better, Faster, Stronger, Dr. Julie Silver, a specialist in rehabilitation and physical medicine at Harvard Medical School and a breast cancer survivor, writes that the three most important physical aspects of a healing lifestyle are:
1. Exercising regularly in a manner that builds strength and endurance
2. Eating a healthy diet
3. Obtaining proper rest during the day (by pacing yourself) and at night (by sleeping well)
Silver advocates making exercise a regular part of your life in order to derive its many benefits: less fatigue, reduction in pain, more strength, improved self-image, enhanced immune function, and decreased risk of developing cancer, among others. Ask your oncologist about resources in your community (such as physical therapy programs and nutrition counseling), and so that you can achieve the three essential physical aspects of a healing lifestyle.
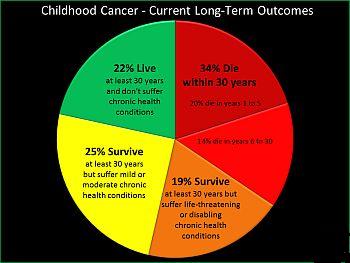
The second aspect of physical recovery involves coping with specific problems wrought by cancer treatment. Surgery may have resulted in new physical limitations that may benefit from a consultation with a physiatrist (doctor specializing in rehabilitation medicine) and a program of physical therapy. Cancer-fighting medications and radiation therapy may have long-term effects on different body systems, including the health of the heart, bones, brain (cognitive impairment), nerves, and reproductive organs (sexual dysfunction and infertility). You will be informed of these potential side effects both before and especially after treatment, when any preventative measures and a schedule for monitoring these systems (such as a bone density test to assess bone strength) are laid out in your post-treatment care plan. Your primary care physicians and other specialists should also be involved in the post-treatment recovery plan. Several resources listed in appendix 2 discuss in detail the possible long-term side effects of cancer treatment.
Monitoring for recurrences or new cancers. The last thing you want to hear out of the mouth of the oncologist after finishing cancer treatment is, “Well, now it’s time for that screening colonoscopy!” Many an oncologist has received a look in response that basically says, “Go jump
in the lake!”
Monitoring for a cancer recurrence and for new cancers that can affect all people is an important component of survivorship. Monitoring (also called surveillance) serves two purposes: (1) to try to detect any developing cancer at its earliest stage; and (2) to help alleviate the concern over recurrences that all survivors experience. Your survivorship care plan will include both routine cancer screening tests, such as colonoscopy, mammography, and PSA measurements, as well as specialized tests (such as CT scans and MRIs) to detect a recurrence of the cancer just treated. The guidelines for cancer monitoring often change, so this aspect of your care plan may need to be updated from time to time.
(71) General Cancer
3D Medical Animation - What is Cancer?

PSYCHOLOGICAL (EMOTIONAL) CHALLENGES
Your psychological state in each stage of survivorship will be different. When initially diagnosed, one must deal with fear and, in some cases, shock and disbelief. At this time, efforts are aimed at developing a treatment plan, a plan of action to survive the cancer. During treatment, the focus shifts to surviving the side effects and trying to be positive and hopeful. If treatments continue for a prolonged period, one must adjust one’s body and mind, make the cancer center a second home, and cope with the chronic side effects of therapy. If treatment is finite, then on its completion, the cancer survivor will work to resolve side effects or adjust to the “new me”; the focus will turn to regaining one’s life and trying to reestablish normality.
Perhaps the most dominant psychological issue facing cancer survivors is the fear of recurrence. Not infrequently, oncologists receive worried phone calls from patients who have completed treatment but who feel a new breast lump, lymph node, or symptom reminiscent of when the cancer began. These fears are normal, and it is our job to provide reassurance (and examinations if needed). Anxiety over a recurrence can never be fully alleviated, but it can be contained.
Some ways to manage it are:
1. Try to live more “in the moment” and not excessively preoccupy your mind with thoughts of what was or what may be (practical preparation for the future is of course important). In an inspiring little book called The Precious Present, by Spencer Johnson, MD, we are all reminded to look around and appreciate what life has to offer today, for this is the path to true contentment.
2. Pursue professional counseling with therapists familiar with cancer issues.
3. Counsel another patient who is going through something you may have experienced (peer-to-peer counseling). You may gain a sense of control that is empowering and feel good that you are helping another person through cancer. Peer counselors need to be trained by professionals in order to provide this kind of support to another patient.
4. Gain as much knowledge and understanding of the cancer as possible so that you can focus on the known facts rather than exaggerated fears of recurrence.
5. Use images to practice guided imagery and focus on the cancer being eradicated or staying away.
6. Separate the anxiety of cancer from anxiety caused by other aspects of your life and seek solutions to those.
The emotional or psychosocial issues generated by cancer are numerous.
Distress and anxiety is universal; feelings of isolation and depression are common. How should you best handle these?
Sometimes medications may improve symptoms, so you should not hesitate to take prescribed antidepressant or antianxiety medications, which may only be needed for a limited time.
Always the solution involves people. Family, friends, and loved ones sustain us throughout life and especially when we are dealing with cancer. Yet you should also seek out other patients and experienced professionals who are familiar with the emotional toll of cancer. Seeking guidance from oncology-trained psychiatrists, social workers, and psychologists, family therapists, and spiritual or religious advisers will lessen your burdens. It is also beneficial to seek out others who arecoping with cancer, because they understand what is happening to you in a unique way. There are many committed and caring people whose job and purpose is to help those with cancer cope from day to day. Yet you must reach out for help or accept assistance when it is offered.
Many cancer patients and their loved ones can benefit from individual or family counseling. Counseling may be limited and used as a bridge until life becomes more normal again or for an extended period.
Whether you need simply to talk about your fears or release the stress that may be interfering with a relationship, counseling can start the healing process and avoid letting negative feelings fester and remain unresolved.
Oncology counselors are familiar with both the stress created by cancer and the range of family dynamics. Counselors are available at cancer centers as well as through other organizations.
One of the best places to find cancer survivors at all stages of the journey is in a cancer support group. You may be reluctant to join such a group. Usually, such reluctance stems from a range of concerns, one of which is a misconception of what a group has to offer. According to oncology social worker Joan Hermann, “Many prospective group members worry that they will hear sad stories and become depressed when what they need is to feel positive and upbeat about their future. While they certainly may hear about the challenges people are experiencing in controlling their cancer, members can also be inspired by the courage and tenacity of others.”
Group leaders at our cancer center, LCSW (licensed clinical social worker), and LMFT (licensed marital and family therapist), liken the experience of joining a group to “the story of the person sitting alone in a boat in the middle of a foggy lake only to discover when the fog lifts, that hundreds of other boaters are all around him.” The support group tackles such issues as how to relate to a spouse, child, coworker, or friend; how to summon the energy to work; how to survive when you can’t go to work; how to communicate with your doctors; and whom you can count on during these difficult times. The experience is often educational and very rewarding as special bonds are formed.
Survival Is Spelled LMNOP
I convey an understanding of cancer in order to promote an enhanced sense of control over a disease known for the lack of control it creates. I also indicate how diet, exercise, and lifestyle can influence the chances of developing and surviving the disease. The five major elements of preventing and surviving cancer can be easily remembered by thinking, “Survival is spelled ‘LMNOP.’”
LMNOP
L is for Less fat in one’s diet
M is for More fruits and vegetables
N is for No Smoking
O is for Organize your life
P is for Physical exercise
O IS FOR ORGANIZE YOUR LIFE
Organize your treatment. Choose caregivers whom you like and trust. Choose a treatment center that fits with your practical needs (such as location) as well as your preferences (for example, a community versus large hospital atmosphere). Get a second opinion when recommended by your primary oncologist or for peace of mind; the more life threatening a cancer, the greater the need to hear more than one opinion.
Choose one oncologist to be your most trusted adviser and ally to help you make the best decisions at every juncture of your cancer journey; you should feel that you have good and open communication with this physician.
Pay attention to new advances reported in the media and on reliable web sites and discuss these with your doctors. But don’t continually second-guess your treatment plan (or let others do so) or bounce from one specialist to another.
If possible, rely on a small group of about three close friends or family members, at least one of whom will be available to accompany you to each treatment.
Organize your loved ones. On hearing the word “cancer,” you will think of yourself and you will think of your loved ones. You will immediately wonder how your spouse or significant other, children, siblings, and parents will handle the news. For the sake of everyone involved, seek the counsel of professionals on how to communicate effectively with your loved ones about your situation. The people in your life may also need the emotional support of a professional counselor at some point. The more united your loved ones are behind you, the stronger you will be throughout your ordeal with cancer.
Address advance health care directives through a living will and a power of attorney document so that your wishes will be respected in the event that you will not be able to direct them (a combination document called Five Wishes is available at www.agingwithdignity.org , but be aware that not all states recognize this document).
Organize your support system. You will need the sturdy support of good friends and loved ones to cope with cancer. Rather than having family and friends give you well-meaning but often overwhelming and distracting advice about what you should and should not do to fight cancer, give them concrete suggestions about how they can show their support. Ask that they help in taking care of household chores, meals, child care, transportation to and from treatment, and anything else you may need to help make your life flow smoothly during and after the grind of cancer therapy. Suggest gift certificates to places that you enjoy (you are entitled!).
Organize your mind. Long-term cancer survivors uniformly state that trying to maintain a positive mental attitude is essential to their survival. But there will be down times, both physical and mental, and it is okay to give into them for limited periods. As my mother used to say to me,
“Only a fool is happy all the time.” Don’t let others badger you to be positive and upbeat around the clock, as this will probably only prevent you from expressing your true feelings, leading to worse depression. So surround yourself with people who truly care about you and know how you like to communicate. Reduce stress in your life as much as possible and minimize interactions with negative people so that you can focus on the critical task at hand. Pursue spiritual and religious tranquility.
Take advantage of hobbies, music, art, yoga, and other activities and techniques to promote relaxation and peace of mind. Celebrate good results. Laugh as much as possible.
Organize your work. You and your employer will want to know how much time you will need to deal with cancer. You may need to work parttime or perhaps sometimes from home, if that is feasible. If arduous treatments are necessary, consider short-term and long-term disability, and know the pros and cons of these. Do not try to maintain a full work schedule and go through rigorous cancer treatments; you will more than likely end up exhausted, compromising both your work and your treatment.
Organize your finances. First, make sure that your medical insurance will cover the prescribed treatments. Your oncologist’s office will be able to verify this. Avoid hospitals that are out of your insurance network unless it is essential that you receive care at such a facility; in these instances, letters from your doctors on the necessity of such treatment usually results in insurance coverage. Second, if you are the breadwinner in your family, make certain that your loved ones will be provided for through clear documentation. Even if you are highly likely to survive your cancer, the diagnosis is a good time to get your financial situation in order.
Organize your time. The ultimate goal is for you to have your life so organized that you can deal with cancer treatment almost on autopilot. This will also enable you to have time for yourself, which is an essential component of the recovery process. Once you have taken control of your life as a cancer patient, you will likely never return to taking each day and the gift of life for granted.
I wish to share with you the inspiring wisdom of two special individuals.
Elizabeth April-Fritz survived a diagnosis of breast cancer in 1998, a recurrence in 2000, and a second recurrence in 2004 that requires continuous treatment. She writes, “I have learned to share my experience with other people, those who have been diagnosed with cancer and those who are caregivers. I am encouraged to share my learning, my philosophy, my appreciation for life. Each day an anniversary . . . each day a gift. It is amazing to realize that as I write these words and date this submission that it is in fact the eight-year anniversary to the day that
I found the original lump in my breast. Eight years later much stronger and wiser and filled with the promise of living life to the fullest.”
And from Patricia Taylor, spouse of a colon cancer survivor:
We all share the need to survive,
To remain alive,
To exist,
To carry on despite hardships,
To persevere.
We want to stay usable,
To cope with what we’re dealt,
To help each other out,
To retain our humanity,
To make some sense of it.
It may not be anything
It won’t replace the life
Broken by cancer,
Like a plate that fell.
And someone hands it back to you,
Saying, “We may be able to put this back together.”
(Or maybe not.)
And once together, never again the same.
But it is something.
Cracks and everything.
Look-In the end,
And through it all,
Much of what we have
Is simply each other.
(72) General Cancer
The Future of Breast Cancer Diagnosis and Treatment
BREAST CANCER SCREENING DIAGNOSIS AND TREATMENT
More Information
1. The Diagnosis and Treatment of Cancer
• Visit the resource room of your local cancer center to find educational booklets on the specific cancer you are interested in.
• Call the Cancer Information Service at 1-800-4-CANCER and request information (this service is sponsored by the National Cancer Institute).
• Visit the National Cancer Institute’s (NCI) web site at www.cancer.gov.
• Go to the American Society of Clinical Oncology’s patient-oriented web site at www.cancer.net
• Visit the Leukemia and Lymphoma Society’s web site at www.leukemialymphoma.org.
• Go to the American Cancer Society’s web site at www.cancer.org
2. Patient Advocacy and Survivorship Groups
Note: These are composed mainly of cancer survivors and other volunteers who provide information, inspiration, and more.
• Visit the Association of Community Cancer Centers’ web site at www.accc-cancer.org
and click on “Patient Advocacy Groups” to find the groups most relevant to the cancer you are interested in.
• Go to the National Coalition for Cancer Survivorship’s web site at www.canceradvocacy.org
• Visit the Lance Armstrong Foundation’s web site at www.livestrong.org.
3. Patient and Family Support Services
• Inquire at your local cancer center about individual or group therapy and counseling for cancer patients and their loved ones (children, spouses, significant others).
• CancerCare at www.cancercare.org provides free counseling, information, and financial assistance to patients.
• The Wellness Community at www.thewellnesscommunity.org provides counseling and educational programs across the
• The National Hospice and Palliative Care Organization at www.nhpco.org explains hospice and enables you to find hospice agencies in your region.
• The Visiting Nurse Associations of
• Go to www.accc-cancer.org and click on “Cancer Care Resources.”
• Visit the web sites listed under 1 and 2, above.
4. Clinical Trials
Note: Only some of the trials available at any cancer center are listed on the Internet.
• Ask your oncologist or the research nurses at your local cancer center about clinical trials at that location.
• Go to the web sites of the different cancer centers in your area.
• Visit the National Cancer Institute’s web site at www.cancer.gov to find information about participating in a clinical trial and to access the largest nonprofit database of trials in the
• Go to www.emergingmed.com , which helps match patients to appropriate clinical trials.
• Visit the TrialCheck web site at www.CancerTrialsHelp.org for the most up to-date information on cancer clinical trials.
5. Genetic Testing for Cancer Susceptibility
• Inquire at your local cancer center about genetic testing or contact the National Society of Genetics Counselors at www.nsgc.org for a listing of genetics counselors in your area who specialize in cancer.
• Go to the interactive government web site http://www.cancer.gov to learn about your personal risk factors for developing cancer.
• Visit www.facingourrisk.com to determine your risk of breast and ovarian cancers.
• Go to www.cancer.net to learn more.
6. Nutrition, Exercise, and Cancer
• Visit the American Institute for Cancer Research’s web site at http://www.aicr.org/ for up-to-date information and resources.
• Go to Cancer Nutrition Info at www.cancernutrition.com/ for sound nutritional advice during and after treatment.
• Consult the book Eating Well, Staying Well during and after Cancer, by Abby Bloch, PhD, RD, et al. (American Cancer Society, 2003), which contains sound advice without the exaggerated claims of many “nutrition and cancer” books.
• Consult the book After Cancer Treatment: Heal Faster, Better, Stronger, by Julie K. Silver, MD ( Johns Hopkins University Press, 2006).
• Visit the web sites listed under 1 and 2, above.



































